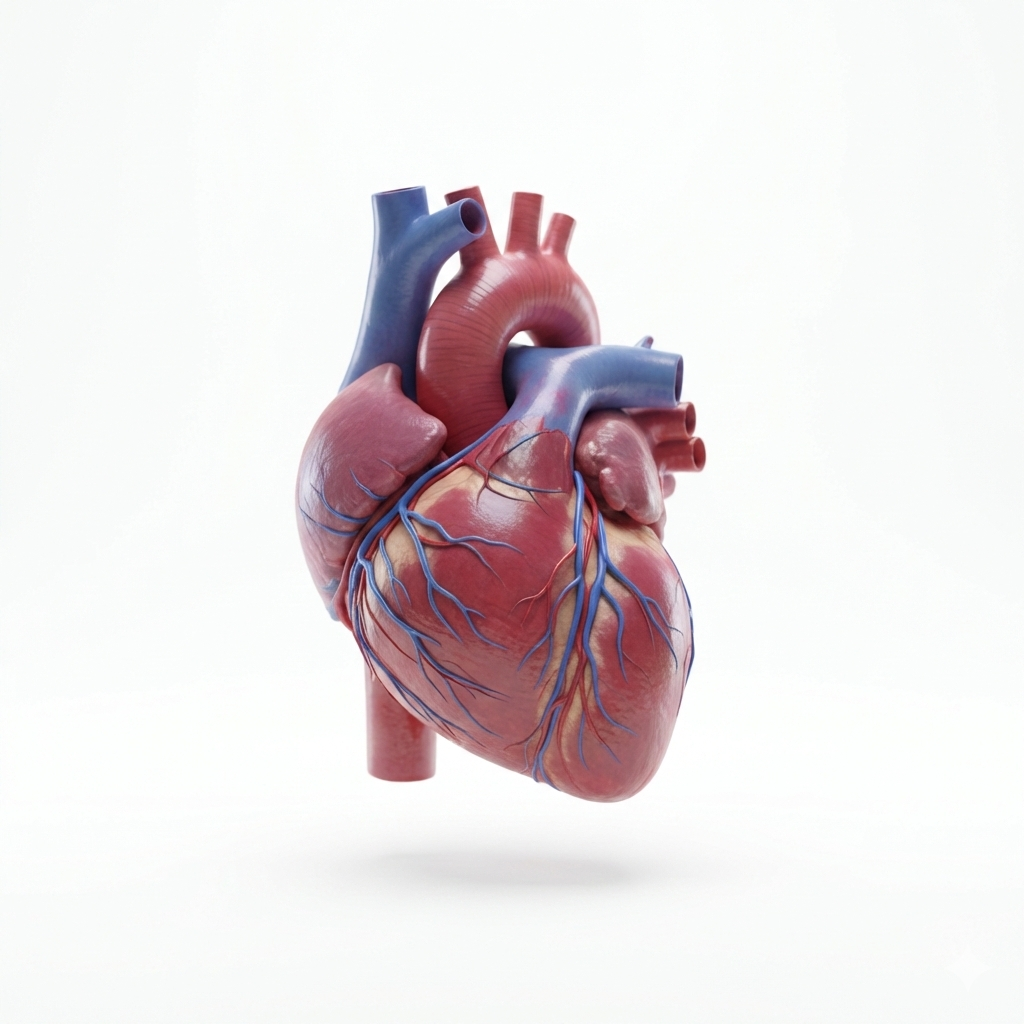
Heart Complications
The heart functions much like a finely tuned machine. It depends on specific nutrients to operate properly—just as a small engine requires the correct fuel mixture, or a car relies on the proper balance of fuel, oil, and coolant to run efficiently.
When a machine lacks one of these essential components, it may appear broken when, in reality, it is simply not receiving what it needs to function correctly. Likewise, if the wrong substance is introduced—such as pouring oil into a gas tank—the vehicle has been filled, but not with what it was designed to use. The result is malfunction, not true mechanical failure.
The same principle applies to the body. If the heart is deprived of essential nutrients or burdened with substances it cannot properly utilize, its performance may become impaired. This can present as palpitations, tachycardia, bradycardia, arrhythmias such as atrial fibrillation (AFib), and in some cases worsening of underlying valve dysfunction.
Optimal cardiac function depends not merely on having “something” present, but on having the right components in the right balance.
Nutritional Influences on Cardiac Function
Certain vitamins and minerals play direct roles in electrical conduction, muscle contraction, oxygen delivery, and vascular integrity.
Vitamin B1 (Thiamine) Deficiency
Mechanism:
Thiamine is essential for mitochondrial energy production (ATP). Because the heart is highly energy-dependent, inadequate thiamine impairs its ability to generate sufficient energy.
Without adequate thiamine:
The heart muscle weakens
Peripheral vasodilation occurs
Fluid retention develops
Cardiac output may initially increase, then eventually decline
Condition: Wet beriberi
Potential Complications:
Dilated cardiomyopathy
High-output heart failure
Edema
Tachycardia
This deficiency is most commonly seen in severe malnutrition, chronic alcoholism, prolonged vomiting, or after bariatric surgery.
Vitamin B12 Deficiency
Mechanism:
Vitamin B12 deficiency can lead to megaloblastic anemia, resulting in reduced oxygen delivery to tissues. To compensate, the heart increases its workload by:
Raising heart rate
Increasing cardiac output
Possible Outcomes:
Cardiac enlargement
Heart failure (if severe or prolonged)
Arrhythmias secondary to hypoxia
B12 deficiency also elevates homocysteine levels, which may increase long-term cardiovascular risk.
Vitamin D Deficiency
Mechanism:
Alters calcium regulation
Contributes to vascular stiffness
Is associated with hypertension
May promote left ventricular hypertrophy
It is important to note that the relationship between vitamin D deficiency and structural heart disease is largely associative rather than definitively causal.
Electrolyte Considerations
Although not a vitamin, magnesium is critical for maintaining normal cardiac electrical stability.
Low magnesium levels may result in:
Arrhythmias
Prolonged QT interval
Increased risk of ventricular tachycardia
Magnesium deficiency is often associated with malnutrition, chronic illness, or gastrointestinal disorders.
Caloric Deficiency and Severe Undernutrition
In prolonged caloric restriction—such as in anorexia nervosa or famine—the heart itself can undergo structural changes.
Mechanisms include:
Cardiac muscle atrophy
Reduced left ventricular mass
Electrolyte imbalances
Lowered blood pressure
Potential Complications:
Bradycardia
Hypotension
Arrhythmias
Sudden cardiac death, particularly from electrolyte disturbances
In severe undernutrition, the heart can become smaller and weaker.
Additionally, refeeding syndrome—when nutrition is rapidly reintroduced—can trigger dangerous electrolyte shifts, particularly low phosphorus and magnesium, which may precipitate life-threatening arrhythmias.
Mechanical and Postural Influences
Mechanical factors may also influence cardiovascular function. Overactivity or compensation in muscles such as the scalenes, neck extensors, diaphragm, or pectoral muscles can affect posture, breathing mechanics, and thoracic dynamics. In some cases, muscular tension patterns may influence autonomic regulation or contribute to altered blood flow dynamics.
These changes may be associated with symptoms such as shortness of breath, fluctuations in blood pressure, palpitations, or lightheadedness. It is important, however, to evaluate these symptoms comprehensively to rule out primary cardiac or vascular disease.
At Healing with Excellence, we utilize a thorough health intake process, your personal health history, laboratory data, lifestyle assessment, and a Neuromuscular Restoration™ evaluation to develop a personalized care plan. Our approach is designed to support cardiovascular health, improve overall function, and help prevent progression where possible.
We are committed to collaborating with you and your medical team to ensure a comprehensive wellness strategy focused on improving quality of life. Our goal is to advocate for you during challenging times—helping reduce stress, uncertainty, and fear while empowering you with clarity and support.